How to Reduce Denials in Medical Billing
How to Reduce Denials in Medical Billing
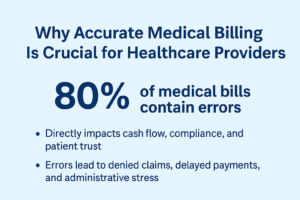
Medical billing denials are one of the biggest challenges healthcare providers face. A denied claim not only delays payment but also adds extra administrative work, which can impact revenue and efficiency. The good news is that most denials are preventable with the right strategies. In this post, we’ll explore practical ways to reduce denials in medical billing.
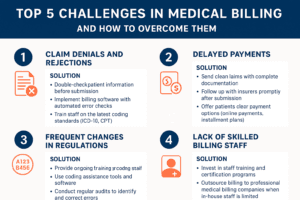
1. Understand the Common Reasons for Denials
Before you can fix the issue, you need to know why claims get denied. The most common reasons include:
Incomplete or inaccurate patient information
Missing or incorrect documentation
Incorrect coding or outdated codes
Lack of prior authorization
Duplicate claims
Services not covered under the patient’s insurance plan
Identifying these patterns helps you target the root causes and avoid repeated mistakes.
2. Verify Patient Information and Eligibility
Errors in patient demographics and insurance details are a leading cause of denials. Always verify:
Patient name, date of birth, and contact details
Insurance policy number and coverage details
Eligibility for the specific service being provided
Conducting real-time eligibility checks before appointments can prevent issues later.
3. Focus on Accurate Medical Coding
Incorrect or outdated codes can easily result in denied claims. To minimize errors:
Stay updated with the latest ICD-10, CPT, and HCPCS codes
Train staff regularly on coding best practices
Use coding software or outsource to certified medical coders for accuracy
Accurate coding not only reduces denials but also speeds up reimbursement.
4. Obtain Prior Authorization
Many payers require prior authorization for certain services or procedures. Failing to secure it often leads to claim denials.
Verify prior authorization requirements before performing services
Document all communications with insurance companies
Use automated tools or tracking systems to manage approvals efficiently
5. Maintain Proper Documentation
Clear and complete documentation supports claims and justifies medical necessity. Providers should ensure:
Detailed patient records
Physician notes aligned with billing codes
Proof of medical necessity
Strong documentation reduces the risk of denials due to insufficient information.
6. Implement a Denial Management System
Even with preventive steps, some denials will still occur. A structured denial management process helps recover revenue faster:
Track and categorize denial reasons
Appeal promptly with corrected information
Analyze trends to improve future processes
The goal should be to learn from every denial and prevent it from happening again.
7. Invest in Staff Training and Technology
Well-trained staff and advanced billing software are essential to reducing denials.
Provide regular training sessions on payer guidelines and billing updates
Use medical billing software with claim scrubbing features
Automate routine tasks like eligibility checks and coding assistance
This combination of technology and human expertise can significantly reduce errors.
Final Thoughts
Denials in medical billing are costly, but they are not inevitable. By verifying patient details, coding accurately, securing prior authorizations, and maintaining strong documentation, healthcare providers can minimize denials and improve revenue cycle performance. Consistent training and the right tools further strengthen this process.
Proactive denial management not only reduces lost revenue but also improves patient satisfaction by ensuring smoother billing experiences.