The Impact of Incorrect Coding on Revenue Cycle Management
The Impact of Incorrect Coding on Revenue Cycle Management
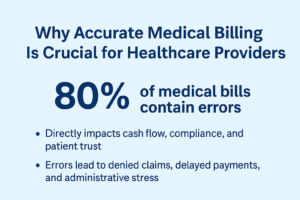
In the healthcare industry, accuracy is everything—especially when it comes to medical coding. Coding errors may seem minor, but they can have a significant impact on a healthcare organization’s revenue cycle management (RCM). From claim denials to delayed reimbursements, incorrect coding not only affects financial performance but can also damage patient trust and compliance with regulations.
What Is Revenue Cycle Management?
Revenue cycle management (RCM) is the financial process that healthcare providers use to track patient care—from initial registration and appointment scheduling to the final payment of a balance. Coding plays a critical role in this cycle, as it translates diagnoses and treatments into standardized codes for billing and reimbursement.
When coding is accurate, claims are processed quickly, and reimbursements flow smoothly. However, even small mistakes in coding can disrupt the entire cycle.
How Incorrect Coding Impacts RCM
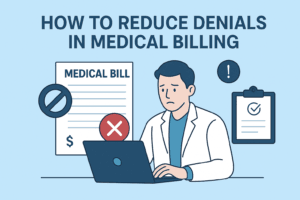
1. Increased Claim Denials
Insurance companies carefully review claims for coding accuracy. Incorrect codes can trigger automatic denials, forcing providers to spend additional time and resources on corrections and resubmissions. This delays cash flow and can cause significant financial strain.
2. Delayed Reimbursements
Even if a claim is not denied outright, coding errors often lead to prolonged verification processes. Payers may request additional documentation or clarification, resulting in payment delays that affect the provider’s financial stability.
3. Compliance Risks and Penalties
Incorrect coding isn’t just a financial issue—it’s also a compliance risk. Repeated errors may raise red flags with regulatory agencies, potentially leading to audits, fines, or even legal consequences for fraudulent billing.
4. Increased Administrative Burden
Every coding mistake adds more work for the billing and administrative teams. Staff must investigate denials, correct errors, and resubmit claims, all of which divert valuable time away from patient care and operational efficiency.
5. Patient Dissatisfaction
Errors in coding can sometimes lead to inaccurate patient billing. Patients may be overcharged or billed for services not received, causing frustration and loss of trust in the healthcare provider.
Common Causes of Incorrect Coding
Lack of proper training for coding staff
Outdated coding systems or software
Complexity of coding guidelines (ICD-10, CPT, HCPCS, etc.)
Time pressure leading to rushed entries
Poor communication between clinical staff and coders
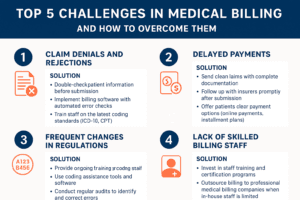
Strategies to Prevent Coding Errors
To reduce the negative impact of incorrect coding on RCM, healthcare providers can:
Invest in ongoing coder education and training
Use advanced coding software and automation tools
Conduct regular audits and compliance checks
Improve documentation accuracy from physicians
Foster strong communication between clinical and billing teams
Final Thoughts
Incorrect coding may appear to be a small problem, but in reality, it creates a ripple effect across the entire revenue cycle management process. By focusing on accuracy, training, and technology, healthcare organizations can minimize errors, improve cash flow, stay compliant, and enhance patient satisfaction.
Accurate coding isn’t just about billing—it’s about building a stronger, more efficient healthcare system.